
In approximately 40% of cases, the retrograde P wave is observed in the terminal portion of the QRS complex. Most commonly (in approximately 50% of cases), the P wave is buried in the QRS complex and is not seen. Regardless of the mechanism, because the tachycardia originates within the AV junction, the atria and ventricles are activated simultaneously. In rare circumstances, a site within the AV node fires rapidly as a result of increased automaticity. In some cases, a premature atrial contraction can block one of the pathways (usually the fast pathway), conduct down the slow pathway, and activate the fast pathway retrogradely, initiating a reentrant circuit.
Usually, one of the pathways has relatively rapid conduction properties but a long refractory period (“fast pathway”), and the other has slow conduction and a short refractory period (“slow pathway”). In AVNRT, two separate parallel pathways of conduction are present within junctional and perijunctional tissue. Junctional Tachycardia: The most common type of tachycardia to arise from tissue near the atrioventricular junction is AV nodal reentrant tachycardia (AVNRT).In some situations, very rapid ventricular rates can be observed due to 1:1 conduction, or slower rates observed due to 3:1 conduction.
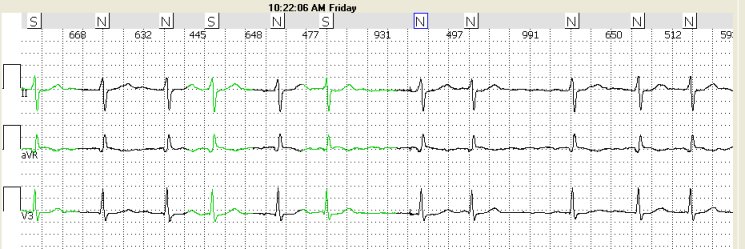
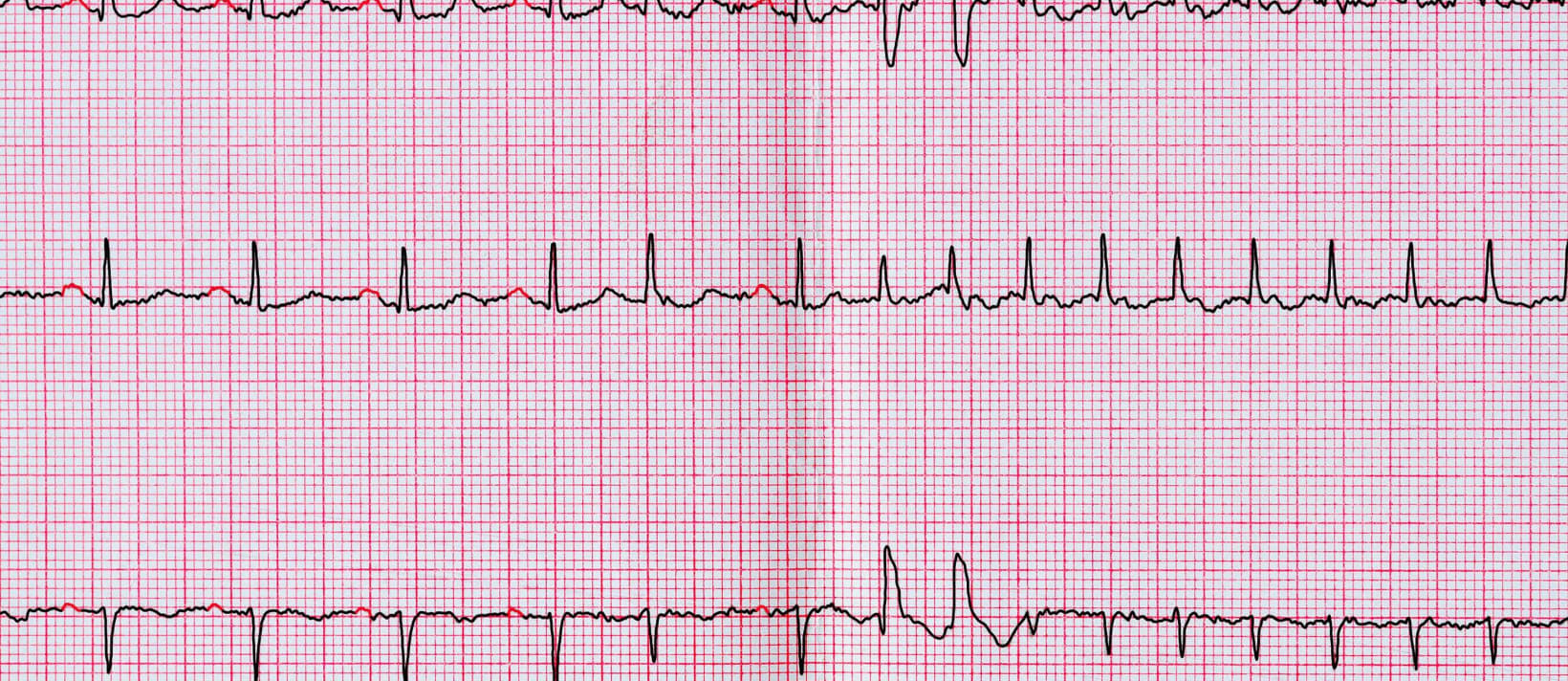
Most commonly atrioventricular conduction occurs with every other flutter wave (2:1 conduction), leading to a heart rate of approximately 150 bpm. Atrial Flutter: The mechanism for atrial flutter is described above.As the atrial tachycardia rate increases, the AV node conduction slows (decremental conduction) and the PR interval increases decremental conduction properties of the AV node prevent rapid ventricular rates in the presence of rapid atrial rates. The PR interval depends on how quickly atrioventricular conduction occurs. The specific shape of the P wave depends on the specific site of atrial tachycardia. This leads to an abnormally shaped P wave. Atrial Tachycardia: Rarely, a single atrial site other than the sinus node fires rapidly.The PR interval is usually relatively normal, because conditions associated with sinus tachycardia (most commonly sympathetic activation) also cause more rapid AV conduction. In sinus tachycardia, an upright P wave can be observed in II and aVF and an inverted P wave is observed in aVR. Sinus Tachycardia: Under many physiologic conditions, the sinus node discharges at a rate >100 bpm ( Figure 7–2).Narrow QRS Tachycardia with a Regular Rhythm: Regular SVT Ectopic Atrial Rhythm Ectopic Atrial Rhythm In children and young adults, sinus arrhythmia (sinus rates that vary by more than 10% during 10 seconds) due to respiration is frequently observed. During sleep, when parasympathetic tone is high, sinus bradycardia (sinus rates 100 bpm) is common. The normal sinus rate is usually between 60 and 100 bpm but can vary significantly. In lead V I, the P wave is usually biphasic with a small initial positive deflection due to right atrial activation and a terminal negative deflection due to left atrial activation. Because the sinus node is located at the junction of the superior vena cava and the right atrium, in sinus rhythm the atria are activated from “right to left” and “high to low.” The P wave in sinus rhythm is upright in lead II and inverted in lead aVR. The sinus node is the primary pacemaker for the heart. Using the categorization above, refer to Tables 7–1 and 7–2 to select a specific diagnosis for the cardiac rhythm. What is the “rhythmicity” of the QRS complexes (defined as the spacing between QRS complexes)? Regular or irregular? (Any change in the spacing of the R-R intervals defines an irregular rhythm.).Is the duration of the dominant QRS morphology narrow (Fast heart rates have fewer than three large boxes between QRS complexes. What is the mean rate of the QRS complexes? Slow (100 bpm): If there are ≥ 17 complexes in a 10-second period, the rate is fast.This method proceeds in three steps that lead to a diagnosis based on the most likely rhythm producing a particular pattern: A rhythm is defined as three or more successive P waves or QRS complexes.Ĭategorize the patterns seen in the tracing according to a systematic method. Most electrocardiograph machines display 10 seconds of data in a standard tracing.

Approach to Diagnosis of the Cardiac Rhythm


 0 kommentar(er)
0 kommentar(er)
